Neurovascular Compression Syndrome
Stratifying Strategies to Relieve Symptoms
There’s more than one way to treat neurovascular compression syndromes and the neurosurgical team at the Weill Cornell Brain and Spine Center bring their skill and experience to all of them.
Neurovascular compression syndromes — hemifacial spasm, glossopharyngeal neuralgia, and trigeminal neuralgia — are generally caused by compression of a cranial nerve due to a redundant or aberrant vascular structure. “Patients can present with either facial pain or hemifacial spasm, the two most common symptoms,” says Philip E. Stieg, MD, PhD, Neurosurgeon-in- Chief at NewYork-Presbyterian/Weill Cornell Medical Center.
Hemifacial spasm results from the anterior inferior cerebellar artery, or a branch, compressing the seventh nerve. “The seventh nerve is responsible for facial expression,” says Dr. Stieg. “Every time the blood vessel abutting the nerve pulses, it causes scarring. Eventually some patients develop spasm, which can be around the eye, forehead, cheekbone, and mouth, or the whole face can be affected.”

Dr. Philip E. Stieg
Patients with hemifacial spasm, generally first seen by a neurologist, are frequently offered botulinum toxin. “The advantage of botulinum toxin is that the patient avoids surgery and it usually stops the spasm,” says Dr. Stieg. “The disadvantage is that if the patient requires repeated injections, the botulinum toxin kills the muscle, so there is a little loss in facial expression and some flattening of facial features. Many patients don’t want to use it long-term because of its secondary effects.”
“The least common presentation is glossopharyngeal spasm, in which patients have brief and recurring attacks of severe pain at the back of the throat, tongue, and/or under the back of the jaw caused by a compression of the ninth cranial nerve,” says Dr. Stieg. “We can prescribe the same medications as for trigeminal neuralgia or perform microvascular decompression. Gamma Knife radiosurgery cannot be used for this condition.”
Treatments for Trigeminal Neuralgia
Trigeminal neuralgia type 1, also known as tic douloureux, is characterized by attacks of intense pain affecting the mouth, cheek, nose, and/or other areas on one side of the face. Type 2 presents with less intense pain, but a constant dull aching or burning pain. Both types of pain can occur in the same individual, even at the same time. In some cases, the pain can be excruciating and incapacitating. “Patients have described it as a lancinating pain, with a sharp, electrical quality as if someone is stabbing a knife or ice pick into their face,” says Dr. Stieg. “Trigeminal neuralgia is usually the result of the superior cerebellar artery compressing the fifth cranial nerve.”
Anticonvulsant medications, such as tegretol, gabapentin, and lamictal, are often used for pain relief for trigeminal neuralgia. “The natural history of this disease follows an undulating course — patients can have terrible pain, it can get better and they can be weaned off medications, and then the pain comes back,” says Dr. Stieg, who adds that some patients do not tolerate medication or it becomes ineffective, in which case they need to go on to another form of therapy.
Gamma Knife stereotactic radiosurgery offers the least-invasive treatment option for patients with comorbidities, high-risk medical illness, or pain that is refractory to prior medical and surgical procedures. “We radiate the root of the nerve as it goes into the brain,” explains Dr. Stieg. “The advantage is that it’s noninvasive; the disadvantage is that one can get facial numbness, and in very rare circumstances patients will describe that facial numbness as facial pain — anesthesia dolorosa — and there is no relief for that.”
Microvascular decompression surgery for trigeminal neuralgia
Peripheral glycerol and alcohol injections provide the next least-invasive treatment modality. Other therapies include percutaneous balloon compression centered at the gasserian ganglion, as well as radiofrequency gangliolysis that involves a selective lesioning of the affected ganglion. “A problem with that approach is if the patient has pain that radiates into the forehead and eye, that’s the area of nerves you want to treat,” says Dr. Stieg. “However, you could numb the patient’s eye and that can be a setup for a corneal abrasion. So, we don’t like to use this therapy in that scenario.”
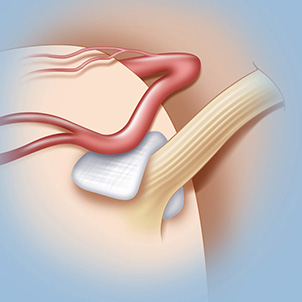
Microvascular decompression is an open surgical procedure that involves moving or removing the blood vessels that are creating pressure on the trigeminal nerve. The neurosurgeon makes an incision behind the ear on the side that is causing pain, exposing the trigeminal nerve, then removes or relocates any blood vessels that are compressing the nerve. “We then slide in a small piece of Teflon-coated felt between the blood vessel and the nerve to relieve pressure from the pulsating vessel pressing on the nerve,” says Dr. Stieg. “If no blood vessels are compressing the nerve, we will perform a rhizotomy to sever the nerve itself. The operation takes three to four hours; the patient wakes up in the operating room and goes home in two days.”
“The beauty of microvascular decompression for younger patients with trigeminal neuralgia is that it’s not destructive, but reconstructive, and our success rate at Weill Cornell is about 90 percent.”
— Dr. Philip E. Stieg
“The beauty of microvascular decompression for younger patients is that it’s not destructive, but reconstructive,” continues Dr. Stieg, adding the success rate with microvascular decompression for trigeminal neuralgia at Weill Cornell is about 90 percent. “For me, it’s a delightful operation because it’s straightforward and patients usually get excellent relief. The approach is also used for hemifacial spasm with a success rate in the mid 80 percent range.”
Of all the treatments, notes Dr. Stieg, radiosurgery offers the shortest duration of pain relief for an average of five years, and radiofrequency lesion has intermittent duration with a 10-year average. Microvascular decompression surgery provides the longest period of relief with an average of 15 years.


