|
|||||||||||||||||||||
Noted Scientist Leads Carroll Laboratories for Orthopedic Surgery On August 1, 2015, Stavros Thomopoulos, PhD, returned to his educational roots with his appointment as Director of the Dr. Robert E. Carroll and Jane Chace Carroll Laboratories for Orthopedic Surgery at NewYork-Presbyterian/Columbia University Medical Center. An internationally renowned scientist, Dr. Thomopoulos earned a Bachelor’s degree in mechanical engineering from Columbia University, followed by Masters of Science degrees in both mechanical engineering and biomedical engineering from the University of Michigan. After a two-year postdoctoral fellowship in biomedical engineering at Columbia University, he went on to serve in a senior faculty position at Washington University. Thirteen years later, Dr. Thomopoulos returned to Columbia, recruited by William N. Levine, MD, Orthopedic Surgeon-in-Chief, to lead the Carroll Laboratories. “Dr. Thomopoulos is one of the world’s leading tissue engineers, with a particular interest in soft tissue-to-bone interface,” says Dr. Levine. “His specific expertise is the rotator cuff, one of the major unsolved problems in all of medicine and, certainly, within orthopedics. Dr. Thomopoulos’s reputation for multidisciplinary collaborations across multiple schools and departments, including clinicians and developmental biologists, as well as mechanical and chemical engineers, is widely known. In addition, he is well funded by the NIH with several R01 grants. His background and experience lend itself well to our goals of bringing our Department to the highest level possible on both the clinical and translational research fronts.” A key mandate for Dr. Thomopoulos, who also serves as Vice Chair of Basic Research in Orthopedic Surgery and holds a joint appoint-ment in Biomedical Engineering at Columbia, is developing translationally relevant research, significantly augmenting research efforts in tendon mechanics, tendon biology, tissue regeneration, and rotator cuff disease processes. The Carroll Laboratories, which opened in November 2014, is an 8,000-square-foot facility that provides a leading-edge environment for cultivating a multidisciplinary musculoskeletal research center. More than 50 principal investigators with some 60 National Institutes of Health awards are conducting musculoskeletal system-related research spanning the basic, translational, and clinical arenas. “In a sense, I have come full circle back to Columbia, my alma mater,” says Dr. Thomopoulos, who first became interested in orthopedic research as an undergraduate engineer exposed to basic research in the Department of Orthopedic Surgery. “The opportunity to come back as head of the Carroll Laboratories is unique and exciting. The Department has always had a strong commitment to research and a very successful research program through the years. One of Dr. Levine’s long-term goals was to expand the research program – especially in the basic sciences.”
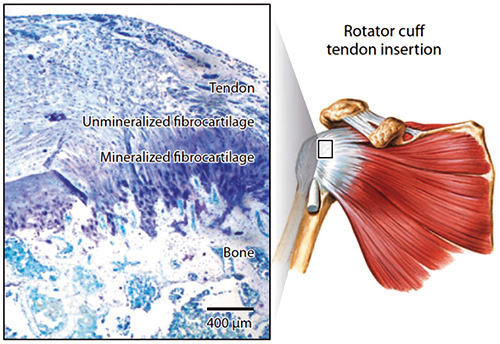
Specializing in the development, structure-function, repair, and tissue engineering of the tendon-to-bone attachment, Dr. Thomopoulos has published numerous papers and authored the book Structural Interfaces and Attachments in Biology on the topic. His research has been funded by the NIH, National Science Foundation, National Aeronautics and Space Administration, and the Orthopaedic Research and Education Foundation. He has received numerous awards, including the YC Fung Young Investigator Award from the American Society of Mechanical Engineers, the Neer Award for Basic Science Research in the Shoulder from the American Shoulder and Elbow Surgeons Society, and the Kappa Delta Young Investigator Award from the American Academy of Orthopaedic Surgeons. Dr. Thomopoulos maintains that the key to a successful research program is establishing close collaborations, noting that he has always felt at home in orthopedics because of his working partnerships with orthopedic surgeons. “When you do basic research, you can often get lost in the details of the science, losing sight of whether the research is clinically relevant,” he says. “Having an orthopedic surgeon involved to advise on the clinical impact is absolutely critical.” As an engineer and a scientist, Dr. Thomopoulos observes that “the fundamental function of bone, tendon, cartilage, and muscle is mechanical in nature, whether you’re considering force generated by a muscle or frictionless gliding of cartilage surfaces. Each function boils down to a very specific mechanical behavior – behavior, by the way, that no engineer has been able to fully replicate in structures or machines.” With this in mind, Dr. Thomopoulos believes that the way forward is biological. “Mechanically, the attachment of tendon to bone is a really interesting problem because you have two very different materials that you’re trying to connect,” explains Dr. Thomopoulos. “The surgeon must connect a rope to a piece of cement and somehow get them to stay together. Over the last few decades, with the design of new suturing methods and devices, the surgical repair mechanics of tendon to bone have improved quite a bit. However, in addition to these mechanical fixation improvements, we need to enhance the biology. The healed tissue not only needs to withstand high loads, but also needs to be continuously maintained and repaired by the local cells in the tissue.” “It’s an incredibly exciting time for our Department and for our field,” says Dr. Levine. “With the generous support of the Carrolls and the leadership of Dr. Thomopoulos, we are poised to take our orthopedic research to the next level.” The Challenge of Attaching Tendon to Bone
Dr. Stavros Thomopoulos and his colleagues are seeking effective biologic solutions to the challenge of attaching tendon to bone from a number of different angles. “To develop successful strategies for tendon-to-bone repair, necessary for rotator cuff repair and anterior cruciate ligament reconstruction, we must first understand the mechanisms by which the healthy attachment transfers load between tendon and bone, and how cells build a functional attachment during development,” says Dr. Thomopoulos. Funded by several NIH R01 grants and one NIH U01 grant, integrated investigations are expected to provide new strategies for enhancing tendon-to-bone repair. These include:
Optimizing Patient Care through Quality, Safety, and Value Initiatives Quality, safety, and value — a triad of related and interdependent components — together form the fundamental basis of providing optimal patient care. This is the precept that drives the work of Michael G. Vitale, MD, MPH, Chief Quality Officer for the Department of Orthopedic Surgery at NewYork-Presbyterian/Columbia. Dr. Vitale, in collaboration with William N. Levine, MD, Orthopedic Surgeon-in-Chief, and Kevin Wang, Quality Officer for Columbia Orthopedics, is vigorously pursuing the development of protocols and processes that will improve the overall outcomes of patients who seek out orthopedic care. “I have long had an interest in quality, but had been primarily focused on pediatric orthopedics,” says Dr. Vitale, who is also Chief of Pediatric Spine and Scoliosis Surgery at NewYork-Presbyterian/Morgan Stanley Children’s Hospital. In 2013, Dr. Vitale led a nationwide quality effort addressing the variability in perioperative surgical site infection practices following pediatric spine fusion. An expert panel composed of 20 pediatric spine surgeons and three infectious disease specialists from North America, selected for their extensive experience in the field of pediatric spine surgery, developed a consensus-based Best Practice Guideline (BPG) consisting of 14 recommendations for the prevention of SSIs in high-risk pediatric patients undergoing spine fusion. For the purpose of their study, the results of which were published in the Journal of Pediatric Orthopedics, high risk was defined as anything other than a primary fusion in a patient with idiopathic scoliosis without significant comorbidities. “By implementing these recommendations, we immediately had a drop in infection rates to near zero,” notes Dr. Vitale, who was lead author on the paper. “And even years later, we still maintain infection rates in pediatric spine surgery that are as low as anywhere in the country.” Since becoming Chief Quality Officer for the Department two years ago, Dr. Vitale and his Columbia colleagues have taken a multidisciplinary, coordinated approach to improve both adult and pediatric patient care in a number of areas, including pain management. “We recognize that we can do better at communicating to patients about expectations and about responding quickly to people with discomfort,” says Dr. Vitale. “In combination with medical and nonmedical treatment, it is critical that patients have perioperative comfort.” Another safety initiative focuses on radiation exposure. “We are reviewing the rational use of X-rays,” says Dr. Vitale. “While a single X-ray generates a limited amount of radiation exposure, a patient diagnosed as a child experiences radiation exposure that is cumulative. So we’ve paid a lot more attention to ordering as few X-rays as needed, being careful about the timing and dosing, and limiting CT scans.” Achieving high value for patients is another overarching goal of the Department. “Value in health care means making sure that everything we do — what we order, everything we purchase, and every orthopedic implant we use — is appropriate and absolutely needed,” says Dr. Vitale. “We’re also constantly reevaluating the amount of lab work required.” Dr. Vitale also calls on the expertise of Henry H. Ting, MD, Chief Quality Officer for NewYork-Presbyterian, and utilizes the well-established quality and patient safety infrastructure of the Hospital’s Value Institute. “It’s truly a team effort,” says Dr. Vitale. “But it requires a combination of a systems approach – a look at institutional and network and infrastructure issues – as well as some on the ground, front-line work with surgeons. Ultimately it’s the surgeons who are in the position to most quickly effect change.” Dr. Vitale cites the Hawthorne effect — the alteration of behavior by the awareness of being observed — to describe efforts to improve quality, safety, and value. “The reality is that if you observe a situation, it gets better; if you shine a light on a problem, it gets better,” says Dr. Vitale, who regularly meets with the Department’s orthopedic surgical team, providing feedback on data. “We start out every meeting as a group with a safety vignette that’s volunteered by a resident or staff member who shares a concern about patient safety,” notes Dr. Vitale. “Part of my role is to follow up on that concern to prevent that particular incident from happening again. Oftentimes it’s just a matter of awareness by the people who are involved that enables us to correct it. Everyone wants to improve their patients’ outcomes, so once you start showing that there is the opportunity to make improvements in so many areas — antibiotic utilization, prophylaxis for deep vein thrombosis, average time to do an operation, or wait time before a patient enters the OR — it almost universally results in a shift in the right direction.” Dr. Vitale allows that there has been emphasis and focus of attention on improving the quality, safety, and value of care in medical centers across the country. “We are certainly not alone in this; there are a number of centers that have a dedicated and similar infrastructure and focus,” he says. “We learn from each other. If a group elsewhere is doing something that works well, you learn from their experiences. I also try to share our experiences, for better or worse. Fundamentally we have an opportunity to make a difference. We’re all very much on the same team.”
First Annual Spine Summit More than 200 physicians from across the United States gathered for the First Annual Safety in Spine Surgery Summit hosted by NewYork-Presbyterian on February 19th. The meeting highlighted numerous safety and quality advances that are being made in spine surgery, enhancing both adult and pediatric spine safety and optimizing outcomes. Michael G. Vitale, MD, MPH, Chief, Pediatric Spine and Scoliosis Surgery and Chief Quality Officer, Department of Orthopedic Surgery, NewYork-Presbyterian/Columbia, served as Chair of the Spine Surgery Summit. John M. Flynn, MD, Lawrence G. Lenke, MD, and Christopher I. Shaffrey, MD, served as Co-chairs. Sessions included strategies to make spine surgery safer; understanding the tools to enhance quality, safety, value, and throughput; and building a successful spine program. “The healthcare system we practice in can be a challenge, and we can use formal tools and quality science to optimize the environment in healthcare and make errors even more rare,” said Dr. Vitale in a recent interview with Becker’s Spine Review. “The biggest changes have come from looking at the episode of care rather than the surgical treatment. That means developing formal ways to assess risk before surgery and using a multidisciplinary team to ensure indications are appropriate and we are choosing the best treatment possible for any given patient.” To read the full article online, visit http://www.beckersspine. com/spine/item/30244-key-opportunities-to-improve-spine-surgery-patient-safety-dr-michael-vitale.html. Dr. William Levine Named Editor-in-Chief of JAAOS Dr. William N. Levine has been named Editor-in-Chief of the Journal of the American Academy of Orthopaedic Surgeons (JAAOS). “I am humbled and honored to have been named the fifth Editor-in-Chief of JAAOS,” says Dr. Levine. “I have grown up with the ‘yellow journal’ and am excited to build upon what my predecessors created before me.” Dr. Levine has served in various leadership roles at the AAOS, including Deputy Editor of JAAOS from 2007 to 2014. He previously served on the Board of Directors of the American Orthopaedic Society for Sports Medicine and is a past Director of the American Board of Orthopaedic Surgery.
|
|||||||||||||||||||||
|
|||||||||||||||||||||