|
||||||||||||||||||||||
|
Harnessing New Technology and Techniques to Atrial fibrillation is the most common and persistent of arrhythmias affecting up to 2.4 million Americans. The arrhythmia is complicated by increased risk of stroke, palpitations, lightheadedness, shortness of breath, fatigue, and heart failure. Not to mention the discomfort and anxiety that arises in patients who experience frenetic heart beats – paroxysmal or persistent. At NewYork-Presbyterian, a significant array of research is underway with the goal of eradicating atrial fibrillation (AF) in patients by improving the treatment options and attacking AF at its source – a challenge that has been readily pursued by physicians in the Divisions of Cardiology at NewYork-Presbyterian/Columbia University Medical Center and NewYork-Presbyterian/Weill Cornell Medical Center. Mapping, tracking, cornering, and halting the skittering electrical impulses that set off disquieting, and even lethal, cardiac arrhythmias remain the means and now often attained targets in treating and curing patients with persistent atrial fibrillation.
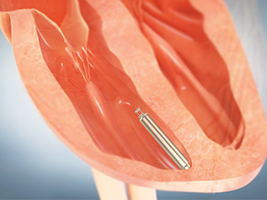
“Appropriate and significant use of high-powered technology in mapping, imaging, and treating many arrhythmias, and especially atrial fibrillation, have infiltrated all phases of diagnosis and treatment,” says Christopher F. Liu, MD, Assistant Director, Cardiac Electrophysiology Laboratory, NewYork-Presbyterian/Weill Cornell. “Determining how to best harness this new technology is based, in part, on how well we can record and process electrocardiograms and electrical signals. It is essential to go beyond displaying patients’ arrhythmia; we also have to be able to effectively map these arrhythmias during procedures. On top of that, we need to treat them using various energy sources.” “In the late 1990s, there was a novel observation that the source of initiation of atrial fibrillation was in the pulmonary veins, which empty into the left atrium,” says Bruce B. Lerman, MD, Chief, Maurice R. and Corrine P. Greenberg Division of Cardiology at NewYork-Presbyterian/Weill Cornell. “Initial data showed that if you electrically isolated each of the four pulmonary veins through ablation, one could achieve cure in about 60 to 70 percent of patients. While this was better than medical therapy, it was still not ideal.” “Basically electrophysiology is still a relatively new clinical science,” notes Hasan Garan, MD, Director of Cardiac Electrophysiology at NewYork-Presbyterian/Columbia. “When we started doing ablations in the 1990s, it became very obvious very early that the more you understood about the circuits that are responsible for the arrhythmia, the more successful the ablation procedure would be.” One of the challenges with atrial fibrillation is that it is not a stagnant disorder – it can progress and one phase changes into another. Prior to recent technological advances, atrial fibrillation’s complex and often transient nature made mapping and tracking its spillover of electrical impulses impossible. “We are now able to collect the electrical activities, or the activation sequence, on a beat-by-beat basis during arrhythmia or at any time,” says Dr. Garan. “In other words, every place in the heart electrically activates and deactivates and waits for the next cycle. With a deflectable catheter that can be navigated from one corner of the heart to the other, you can find out what area, at a given instant, is activating. In the past few years, clinical research has focused on how the atrium activates during atrial fibrillation. Before it just looked like chaotic activity; now patterns are beginning to emerge and the technology is trying to make it possible for us to observe these repeating patterns.” Building on Ablation Technology “With an arrhythmia, there is an initiator – something has to trigger it,” says Dr. Lerman. “But then, in order to sustain the arrhythmia, there needs to be a substrate or perpetuator that allows atrial fibrillation to continue. This is particularly relevant for patients with persistent atrial fibrillation. The electrophysiological substrate is believed to be related to rapidly spinning rotors. These perpetuators are often located in the left atrium; however, in as many as 25 percent of patients, the right atrium may participate. “The rotors cannot be observed with the naked eye,” continues Dr. Lerman, who is the principal investigator for the Randomized Evaluation of Atrial Fibrillation Treatment with Focal Impulse and Rotor Modulation Guided Procedures (REAFFIRM) study. “But now a novel diagnostic catheter and mapping approach allows us, through extensive computerized processing of electrical information, to highlight in a three-dimensional projection the coordinates of the rotors so that we can direct our ablation catheter toward those regions.” The prospective, multicenter, randomized REAFFIRM control trial, which continues to enroll patients, will determine the safety and effectiveness of rotor ablation followed by conventional ablation versus conventional ablation alone for the treatment of persistent atrial fibrillation. Two years ago, Dr. Liu added cryoballoon ablation to his repertoire of techniques for the treatment of atrial fibrillation. “Our goal is to simplify the ablation procedure and improve outcomes. Traditional radiofrequency ablation focuses on pulmonary vein isolation and makes use of a single-point catheter that applies 20 to 25 meticulously placed points, forming a circle around each pulmonary vein. Cryoballoon ablation essentially allows us to go in and freeze the entire circle in one shot.” According to Dr. Liu, this technology streamlines the procedure – shortening the time the patient is under anesthesia and potentially reducing complications. He is now conducting a retrospective study comparing 100 cases of cryoballoon ablations with the same number of cases of radiofrequency ablation, looking at timing, complications, and outcomes, in particular, rates of recurrence of atrial fibrillation. “There are multiple subtypes of atrial fibrillation and as a first step we still perform pulmonary vein isolation,” says Dr. Garan. “The next steps have to be individualized depending on the kind of patient you are treating and/or the subtype of atrial fibrillation. For atrial fibrillation, even with the subtypes that are most amenable to the ablation – young, healthy people who otherwise do not have any structural heart disease – we are at 70 to 80 percent of efficacy. To go to a higher level of efficacy, as we have done with the other forms of arrhythmias where a single ablation can achieve 96 to 98 percent efficacy, there’s still a lot to be learned about down-the-line mechanisms and the different subtypes of atrial fibrillation, as well as the different techniques and methodologies that work best for each. That is why we are still doing clinical investigations in this area.” What You See Is What You Can Get While ablation techniques have been rapidly evolving, visualizing the field has also undergone dramatic growth. “In the past, when we started performing radiofrequency ablations, fluoroscopy was used to visualize the location of the catheter,” says James E. Ip, MD, a cardiac electrophysiologist with NewYork-Presbyterian/Weill Cornell. “Through the years, CT scans or MRI have been utilized to create a road map. Today, we now combine these technologies with intracardiac echocardiography and an electroanatomic mapping system that enable us to pinpoint where we are within the heart.” William Whang, MD, a specialist in heart rhythm disorders with the Division of Cardiology, NewYork-Presbyterian/Columbia, sees patients with atrial fibrillation related to a number of cardiac conditions, including cardiomyopathy and adult congenital heart disease. Similarly, Dr. Whang and colleagues have employed various new imaging and treatment technologies that provide a three-dimensional image of the catheter as it is guided inside the heart, improving the efficacy of radiofrequency ablation. “We use several imaging modalities simultaneously, such as fluoroscopy, intracardiac echocardiography, and electroanatomic mapping,” says Dr. Whang. “I think about electroanatomic mapping as a GPS-type of system where there is a magnet in the tip of the catheter as well as a magnet under the cath lab table. We know at any time where the catheter is in three-dimensional space. This is so we can mark different areas where there’s suspicion for electrical activity that could be helping to maintain or trigger the A-fib.” Dr. Whang and his colleagues create a three-dimensional map of the atrium through a combination of touching the endocardial surface of the atrium with the catheter and integrating this information with the intracardiac echo, as well as a pre-procedure CT scan to reconstruct the left atrium in a three-dimensional form. In addition to new technology permitting greatly enhanced, three-dimensional visualization, Dr. Whang and Dr. Ip each use the most advanced catheter ablation technology, including contact force-sensing (CF-sensing) catheters, enabling them to assess whether adequate contact has been established with atrial tissue at the tip of the catheter. Prior to the availability of the CF-sensing catheter, there was a 20 to 30 percent recurrence rate for atrial fibrillation ablations. “The great challenge,” Dr. Whang says, “is trying to draw a complete line of block in a great many different areas in the atrium. If there’s a gap in the line of block it can jeopardize the entire treatment. The force-sensing technology ensures a complete lesion at each site where we do an ablation.” “Success rates for ablations vary from institution to institution and person to person,” adds Dr. Ip. “But the contact force-sensing catheter has the potential to increase the effectiveness of the procedure across the board.” Waves of the Future
Future progress in understanding atrial fibrillation also lies within the basic laboratories of Columbia and Weill Cornell, with clinicians and scientists seeking to better understand the mechanisms at the core of arrhythmias. Steven O. Marx, MD, Director of the Cardiovascular Fellowship Program at NewYork-Presbyterian/Columbia, and his colleagues have been focusing on arrhythmogenesis in both ventricle and atrial arrhythmias. “All the electrical signals in the heart are generated through ion channels,” says Dr. Marx. “We’ve been studying the mechanisms of regulation of these channels at both the basic science level, as well as in a mouse model. One of the mouse models we produced – somewhat serendipitously and out of the ordinary – is capable of spontaneous atrial fibrillation.” According to Dr. Marx, the standard in the field for studying atrial fibrillation in the mouse model is to induce an arrhythmia of one second, which is reason for skepticism about the value of this model. “One second does not mimic the hours or days a person with atrial fibrillation experiences,” says Dr. Marx. “Because our mouse has atrial fibrillation spontaneously, and it can last for hours, we can monitor and map its electrical patterns. So this mouse model is very useful in figuring out the mechanisms of atrial fibrillation. Why does it stop? Why does it start? Using advanced optical mapping techniques, we have persistent rotors in both the right and left atria of mice, mimicking what is observed in humans. These rotors are the targets in the REAFFIRM study.” Perhaps the only thing Dr. Marx finds more singular than the lab’s serendipitous mice is the human collaboration that creates all these forefront possibilities. “The unique part of this,” Dr. Marx says, “is that it’s a team effort, from both the basic science and clinical aspects of cardiology.” “The mapping of the atrial fibrillation is still being perfected, but for arrhythmias that can be analyzed on a beat-by-beat basis, our techniques are pretty good in enabling us to do successful ablation,” says Dr. Garan. “Atrial fibrillation is still a little elusive and there’s more room for research, debate, and perfection.”
|
||||||||||||||||||||||
|
||||||||||||||||||||||