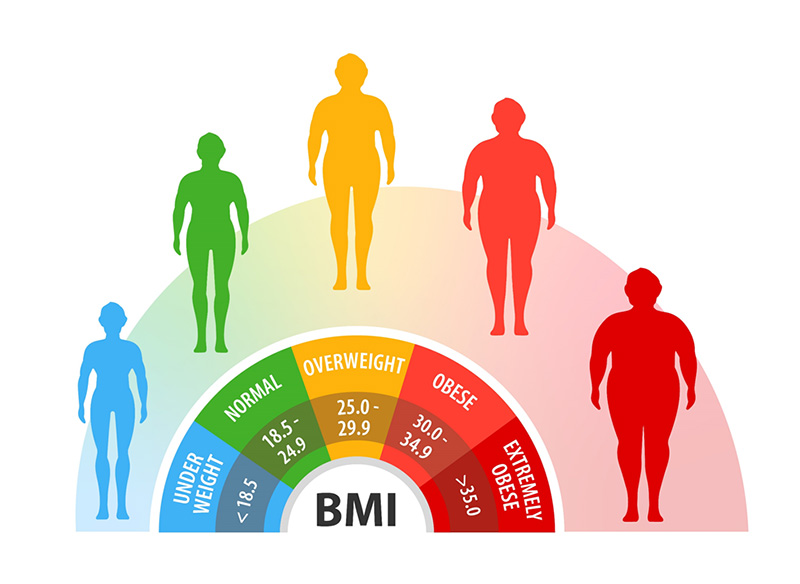
As people with cystic fibrosis (CF) are living longer lives, many will face complex health issues associated with the aging process and with the disease itself, including cancer. Adults with CF have an increased risk of a variety of cancers, especially gastrointestinal (GI) cancers. In CF higher body mass index (BMI) is associated with improved long-term outcomes, yet in the general population high BMI (a marker of obesity) is associated with increased cancer risk.
To better understand the role of BMI and other risk factors for cancer in adults with CF, Julian Adin Abrams, MD, a gastroenterologist and cancer specialist at NewYork-Presbyterian/Columbia, together with other clinician researchers at Columbia University and other institutions, conducted a large retrospective cohort study using data from the CF Foundation Patient Registry. The researchers discovered higher BMI was associated with a reduced, not increased, risk of cancer in adults with CF and a history of organ transplantation. Correspondingly, a lower BMI in transplanted CF patients is associated with an increased risk of cancer. In the field of gastroenterology, this important finding will help shape strategies to optimize the health for people with CF as the treatment landscape continues to evolve.
“Adults with CF are living much longer than in the past due to major advances in medical therapy for this disease,” says Dr. Abrams, a specialist in the care of patients with diseases of the digestive tract including Barrett's esophagus, early esophageal cancer, and other esophageal disorders. “As a result, we have now learned that CF patients have increased risks of a variety of cancers. It is important to understand the risk factors for these cancers in CF patients so that strategies can be developed and implemented to reduce the risk of cancer in this population.”
Cystic fibrosis is a progressive, genetic disease that affects the lungs, pancreas, and other organs. Many patients with CF develop lung dysfunction, and face the possibility of a lung transplant. Patients with CF also have an increased risk of GI cancers, such as cancer of the colon, esophagus, stomach, small intestine and gallbladder. Additionally, the incidence of several cancer types, and colon cancer in particular, is increased among patients who have undergone solid organ transplant.
BMI is another strong determinant of outcomes in people with CF. Although obesity is associated with an increased risk of a variety of cancers and many other diseases in the general population, low BMI in CF patients is associated with worse clinical outcomes. In CF patients, low BMI may be a marker of a chronic intestinal and systemic inflammation, which in turn may predispose them to the development of cancer.
To bridge the knowledge gap in the relationship between BMI and cancer risk in CF, the researchers conducted a retrospective cohort study of adult patients with CF using data collected from the CF Foundation Patient Registry between 1992 and 2015. Additional aims included examining BMI trajectory and examining the relationship between pancreatic insufficiency and pulmonary function (as measured by FEV1) as potential risk factors for cancer in this population. Multivariable logistic regression was performed, with analyses stratified by history of transplant (type of transplant is not specified).
Of the 26,453 adult CF individuals who were identified between 1992 and 2015, 26,199 had cancer data and were included in the analyses. Of those individuals, 3,642 (14.0%) patients had undergone transplant. The study found that increased BMI was associated with a reduced risk of cancer overall in transplanted but not in non-transplanted patients. Additionally, a higher BMI two years after transplant was also associated with a reduced risk of cancer. BMI trajectories over time were not associated with cancer risk. In non-transplanted patients, pancreatic insufficiency was associated with a significant three-fold elevation in cancer risk, and increased FEV1 was also associated with increased cancer risk. Unsurprisingly, older age was associated with an increased risk of cancer in both transplanted and non-transplanted patients. CFTR mutation type was not an independent risk factor for development of cancer.
As gastrointestinal cancers comprise a number of cancers in adults with CF, the authors hypothesize that gut microenvironment alterations may correspond to impaired digestion and absorption with resultant lower BMI, as well as chronic inflammation and increased risks of GI cancer. Thus, in CF patients, higher BMI may correspond with a less “dysbiotic”, or imbalanced gut microbiome, which could explain the observation that overweight and obese CF patients did not have an increased risk of cancer. Similarly, despite the known risks associated with obesity in the general population, there are data suggesting that being overweight or obese may results in better pulmonary function than in normal weight CF patients. Among non-CF patients there appears to be protective effects of obesity with pneumonia survival and lung cancer, known as the “obesity paradox”. The authors suggest this effect may also be playing a role in the CF population.
These research findings contribute important insights to help GI clinicians optimize the care of adults with CF, including those with and without transplant. “Low BMI in CF patients is likely due to factors such as inadequate nutrition, chronic intestinal inflammation, and major changes to the gut microbiome,” says Dr. Abrams. “Strategies aimed at optimizing nutrition, reducing intestinal inflammation, and restoring a healthy microbiome in CF patients may ultimately improve the long-term health of adults with CF.”
The research findings also highlight opportunities for further research regarding the interplay of these risk factors and cancer in CF patients. “Research aimed at correcting these factors may, in the long run, reduce the risk of cancer in CF patients,” says Dr. Abrams. “More research is also needed to understand how these factors influence the risk of specific types of cancers.”
Dr. Abrams is applying his extensive training in cancer epidemiology to unravel the relationship between cancer risk factors to enhance the health and wellbeing of people with CF. “We are in the process of publishing work looking at the relationship between the gut microbiome, bacterial by-products (metabolites), and colon adenomas (precancerous polyps) in patients with CF,” says Dr. Abrams. “This is an exciting field with many discoveries yet to come.”


