|
||||||||||||||||||||||||
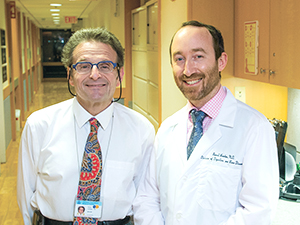
Inflammatory Bowel Disease: Where Do the Answers for Better Treatment Reside? For much of his 30-year career, Simon Lichtiger, MD, Director of the Inflammatory Bowel Disease (IBD) Center in the Division of Digestive and Liver Diseases at NewYork-Presbyterian/Columbia University Medical Center, has studied, and indeed pioneered, new medications for the treatment of inflammatory bowel disease. For the past decade, immunologist David Artis, PhD, Director of the Jill Roberts Institute for Research in Inflammatory Bowel Disease at Weill Cornell Medicine, has pursued studies of the immune system – how it has evolved and operates to fight infection, and how it can become dysregulated in the context of chronic inflammatory diseases, including IBD. Both are world-renowned experts in the field, applying their clinical and basic science perspectives, respectively, to better understand and ultimately treat one of medicine’s most perplexing challenges. “One of the problems that we faced when I started my career was that cortisone was the only effective medication available for IBD – a terrific medication, but with myriad side effects,” says Dr. Lichtiger. “For years we looked for newer medications as a different way of treating IBD. In the 1980s, we had a drug called 6-MP, or 6-mercaptopurine. In the 1990s, we had a drug called cyclosporine. And then, in 1999, there was a new medication that blocked tumor necrosis factor, which turned out to be amazingly effective in IBD.”
According to Dr. Lichtiger, who trained with Daniel H. Present, MD – the first researcher to show the effectiveness of 6-MP in fighting Crohn’s disease – and who also did pioneering work on cyclosporine, “When the new anti-TNFs came out, research became more pharmaceutically driven. In other words, if you had an idea in the 1980s and 1990s, you would take that idea to a company and tell them, ‘I think I have an inkling that this drug may be effective in inflammatory bowel disease.’ With the advent of the anti-TNFs, it became the pharmaceutical companies approaching practitioners to see if they would like to participate in trials of new medications. In the past 20 years, there’s been an explosion of medications, with more and more focused treatments in the pipeline.”
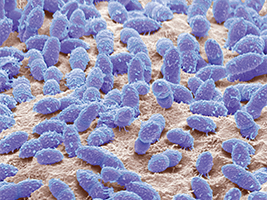
Despite the development of groundbreaking treatments for which Dr. Lichtiger has been an essential driving force, he says, “The Holy Grail lies in understanding the cause of IBD disease. We don’t really know its etiology. In the last decade, the focus on the role of the immune system in IBD has become secondary to studies on the bacterial component of the microbiome. We started to recognize that individuals with IBD have a different microbiome from those who do not have IBD. Is it an initial abnormal immune response, or is there something different about the bacterial contents within their bowel? A lot of this was concomitant with the concept of fecal transplants where, in certain infections, you could do a fecal transplant and the patient would get better. I think that some of the springboard to the microbiome in IBD involves the recognition that feces could be used as therapy. Much research now is directed at trying to isolate the differences in the microbiome so that we’re better able to take care of the disease itself.” Rethinking Microbes: Separating the Bad from the Good “There’s been a real biomedical revolution in our understanding of the relationship the human body has with beneficial microbes that colonize a body’s barrier surfaces,” says Dr. Artis. “Historically, we were all taught that all bugs are bad and we must sterilize everything. Now we know that there are beneficial microbes – the intestines, for example, are colonized by trillions of these beneficial microbes – that are absolutely essential for human health. Changes in the microbiota are now associated with many inflammatory and metabolic diseases, with the indication that a disorganization in the composition of the microbiota may be contributing to the development of diseases such as IBD, asthma, or even cancer and autism. “In inflammatory bowel disease, there are about 170 polymorphisms associated with susceptibility to IBD telling us that there is definitely a genetic component to this disease,” continues Dr. Artis. “Where I think the microbiota comes in is that it is estimated that the healthy microbiota of a human encodes more than 100 times the number of genes that the human genome encodes. So this has provoked a rethink. As we consider genetic susceptibility to disease, it’s not just our own genomes we have to think about, but the microbial genomes that we are partnered with throughout life. Doing the math, we’re into the billions of possibilities.” Dr. Artis suggests that this may explain why in some of the genetic studies – not only in inflammatory bowel disease, but with any human diseases – associations are quite weak, and while there are often polymorphisms that are highly prevalent in the population, only a fraction will develop any given disease. “That always led us to suspect that there’s something going on beyond genetics,” notes Dr. Artis. “The genetic component is obviously very important, but so are environmental and other factors, one of which we think now is the influence of the microbiota. Ultimately, our goal is to understand how these chronic inflammatory diseases develop and to identify how we can determine new therapies to intervene in, prevent, or at least limit the symptoms of these diseases.” From research of the past few years, Dr. Artis notes that it is now known that there are profound changes in the composition of the microbiota in many different diseases. “Those observations – and that’s all they are – tell us that there may also be a microbial component that is influencing diseases with resistance,” explains Dr. Artis. “So, how do we use that information? We can employ microbiologic techniques to isolate individual organisms of the microbiota to study how they influence the immune system, our metabolism, or any aspect of normal physiology. The eventual hope is to identify a healthy microbiota and an unhealthy microbiota that can develop in any given disease state so that we can develop therapies that would restore a healthy microbiota. Whether that comes in the form of probiotics or in the form of drugs that mimic the signals derived from a healthy microbiota is one of the biggest challenges we face. And one of the most exciting challenges, I think, because it has opened up a whole new therapeutic avenue to consider – targeting microbial communities to treat disease.”
Will Treatment for C. diff Point to Treatment for IBD? In 2015, Garrett Lawlor, MD, was recruited to join Dr. Lichtiger in developing the IBD Center at NewYork-Presbyterian/Columbia. Prior to joining the Center as its Associate Director, Dr. Lawlor was the Director of the IBD program at the Brooklyn campus of the Department of Veterans Affairs New York Harbor Healthcare System, establishing a tertiary referral service for veterans in the Northeast suffering from IBD. At the same time, he served as Assistant Director of the SUNY Downstate GI Fellowship Program, where he was doing microbiome research into C. diff infection.
“We know that C. diff-associated diarrhea results as an alteration in the gut’s bacterial content, but we don’t know specifically what the alteration is,” explains Dr. Lawlor. “Therefore, we are unable to prevent C. diff diarrhea from occurring, and we still have to decide among a number of antibiotic therapies that might be most efficacious for a patient. Trying to determine preemptively which patient is going to respond to what antibiotic is difficult. By looking at alterations in the gut microbiome, our hope was to be able to see predictors of response to therapy that could dictate which antibiotic to use to treat the patient.” Dr. Lawlor’s research also involved looking at the efficacy of fecal microbiota transplant in patients who did not recover with antibiotic therapy. “The source of a fecal transplant can either be a known donor, such as a spouse, family member, or friend, or from an unknown donor who has been prescreened,” says Dr. Lawlor. “The first stool bank that made universal donors available was developed in the laboratory of Eric Alm at MIT, and they provided us with healthy stool for the fecal transplant for Veterans while I was with the VA.” The idea behind fecal transplant is to introduce healthy bacterial flora into the patient’s microbiome to displace or overcome the C. diff pathogen. The FDA considers fecal transplant an investigational new drug, but recently issued guidance that it may be used to treat C. diff infection not responsive to standard therapies outside a clinical trial. Its success in treating C. diff has led to consideration of fecal transplant as a novel treatment for IBD. Dr. Lawlor points out, “Our understanding of what causes IBD is rapidly evolving, even on a yearly basis. This is why specializing in the management of IBD is so exciting.” A clinical trial is now underway at the Jill Roberts Center for Inflammatory Bowel Disease at Weill Cornell led by Vinita E. Jacob, MD, and Carl V. Crawford, MD, to test whether a fecal microbial transplant could be an effective way to deliberately try to change the composition of the microbiota and limit inflammatory bowel disease. “Some forms of inflammatory bowel disease, such as C. diff colitis, develop in patients, typically, who are on broad-spectrum antibiotics,” says Dr. Artis. “There’s an outgrowth of a bad microbiota because the antibiotics obviously kill a lot of beneficial microbiota. Most of those patients are refractory to many of the common treatments, but there is a 94 percent efficacy of a fecal microbial transplant reversing their disease. This is better than any drug for any disease that I know of and tells us that, in principle, deliberate manipulation of the microbiota to change its composition could be used as a treatment strategy to prevent diseases like IBD. This is very exciting because it may take us beyond our traditional approaches of dampening inflammation by using fairly non-specific drugs to much more specific therapies that could be microbiomically based.” Advancing IBD Research At Weill Cornell, Dr. Artis and the Roberts Institute team have developed a robust translational IBD effort working with Robbyn E. Sockolow, MD, Director of Gastroenterology and Nutrition at NewYork-Presbyterian/Komansky Center for Children’s Health, and on the adult side, Ellen J. Scherl, MD, Director of the Jill Roberts Center for Inflammatory Bowel Disease. “We have established a unique resource at the Roberts Institute: an IBD live cell bank of samples from patients and healthy controls,” says Dr. Artis. “Every day of the week, we are able to isolate immune cells and study them as well as profile the composition of the microbiota of patients. We now collect blood and biopsies from the diseased intestines and have developed protocols that allow us to viably freeze these immune cells so we can then use them to study IBD and better define its complexity. Coupled with our ability to genotype patients, our hope is that the work that we are doing, in very close collaboration with Ellen and with Robbyn, is to gain a 21st century vision of how the immune system is changed in the context of IBD, how the human genome and microbiotas change, and how we might be able to manipulate those changes to reverse the disease itself.” In collaboration with Peter H.R. Green, MD, Director of the Celiac Disease Center at Columbia, Dr. Lawlor is working on the development of a tissue, stool, and blood bank of samples from patients with IBD, celiac disease, C. diff diarrhea, infections, and other GI disorders. “This will be a remarkable resource for translational research in IBD, enabling us to gain greater understanding of the immunological similarities of these conditions and pursue research to find their triggers,” says Dr. Lawlor. In the meantime, Dr. Lawlor is also very interested in the growing complexity posed by IBD demographics. “There is no question that the incidence and prevalence of IBD is increasing across the board, and increasing more rapidly in minority populations,” says Dr. Lawlor. “Interestingly, we used to say, ‘It’s only about the white population. It’s only about the Ashkenazi Jewish population.’ Now we are seeing a rapid development in the Hispanic, Asian, and black populations.
“One possibility for this identification of IBD in new populations is that it was just never diagnosed properly,” says Dr. Lawlor. “Another is environmental change. Could it be that these populations are being more exposed to the Western diet and therefore to the pathogenic antigens that might be placing people at greater risk of the development of IBD? This is an exciting area of IBD research. For every study looking at the efficacy of a drug or a new prevalence or risk factor, it may be necessary to repeat that 10-fold to look at the differences among ethnicities to fully understand the impact and implication of the data.” With the knowledge that the diseases that comprise IBD are very complex and heterogeneous, and no one therapy is going to suit every patient, Drs. Lichtiger, Artis, Lawlor, and their GI colleagues are hopeful that defining patients by their individual groups of symptoms or individual changes in their microbial communities might allow them to gain much more precision in the way they treat these diseases. “It’s fascinating how a single disease has so many protean manifestations,” says Dr. Lichtiger. “Even with the best medications available, 60 percent of patients are not going to respond to treatment.” “I think this is a challenge of the 21st century,” adds Dr. Artis. “How can we better immunologically, genetically, and microbially profile an individual patient to understand his or her individual disease. I think that’s where we are going to make some very exciting breakthroughs.”
Dr. Timothy Wang to Lead the Timothy C. Wang, MD, AGAF, Chief, Digestive and Liver Diseases, NewYork-Presbyterian/Columbia, has been elected President of the American Gastroenterological Association (AGA), effective May 2016. Dr. Wang, a distinguished clinician, scientist, and educator, has been an active AGA member since 1986 serving on several boards, including the By-Laws Committee, Public Policy Committee, and most recently as Chair of the AGA Institute Research Policy Committee. He has received numerous awards for his contributions to the field of gastroenterology, including the AGA Senior Research Fellow Award and the AGA Robert & Sally Funderburg Research Award in Gastric Cancer. Dr. Wang has served as associate editor for Gastroenterology and GI and Hepatology News, as well as Editor-in-Chief for Therapeutic Advances in Gastroenterology. A prolific researcher, he has published more than 240 peer-reviewed articles, many of which have appeared in Gastroenterology, Science, Nature, Nature Medicine, Cell, and Cancer Cell. Dr. Wang has served as Chief of the Division of Digestive and Liver Diseases at Columbia for the past 12 years. Under his leadership, the Division has grown in numerous clinical areas, including inflammatory bowel disease, GI cancer genetics, and GI motility, and has further expanded the Pancreas Center, Barrett’s esophagus research program, and the Celiac Disease Center. “I am honored to assume the presidency of this prestigious organization, with a diverse membership of some 16,000 clinicians and researchers from around the world,” says Dr. Wang. “I look forward to working with my colleagues to promote the science, practice, and advancement of gastroenterology and address the issues that confront our specialty today.”
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||