The specialists in the Center for Advanced Digestive Care (CADC) at NewYork-Presbyterian/Weill Cornell Medical Center are highly experienced in diagnosing and treating pancreatic cysts and pseudocysts. An interdisciplinary team of gastrointestinal specialists in endoscopy, gastroenterology, radiology and interventional radiology, and surgery works together to provide each patient with coordinated, advanced, and individualized care. Please contact our Advanced Interventional Endoscopy team to discuss your case.
About Pancreatic Pseudocysts
A pancreatic pseudocyst is a collection of pancreatic juice encased in tissue, and develops either inside or around the pancreas. Pseudocysts occur most commonly after an episode of pancreatitis or abdominal trauma. Pseudocysts can be single or multiple, small or large. Depending on the nature of the pseudocyst (size, location, or cause), some will improve on their own, while others require treatment.
Treatment Of Pancreatic Pseudocysts
In some patients with pancreatic pseudocysts, conservative management is appropriate. For instance, if a patient's pseudocyst is small and is not causing any symptoms, sometimes just monitoring the patient is appropriate. In these patients, CADC physicians address nutritional issues, make sure the pseudocyst resolves on its own, and prevent complications. In addition, it is important to determine the cause of the disorder to avoid another episode.
In other patients, however, drainage of the pseudocyst is needed. Drainage is more commonly required in patients with pseudocysts or necrosis (dead tissue) causing symptoms (such as abdominal pain, nausea, vomiting, and difficulty eating), and in those with complications such as infection or bleeding.
In the past, most patients who required treatment for these pseudocysts had to have surgery, but we are now able to drain many of these collections with less invasive endoscopic procedures.
Examples include:
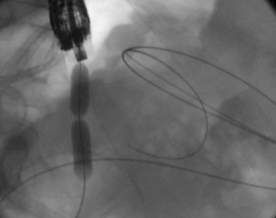
- Echoendoscopy: A stent is used to drain the pseudocyst by connecting it to an adjacent intestinal organ, using an endoscope with an ultrasound transducer at the tip.
- Cystogastrostomy: A connection is created between the back wall of the stomach and the cyst to drain it directly into the stomach.
- Cystojejunostomy: A connection is created between the cyst and the small intestine so that the cyst fluid can drain directly into the small intestine.
- Cystoduodenostomy: A connection is created between the duodenum (first section of the small intestine) and the cyst to allow drainage of the cyst fluid directly into duodenum.
The type of drainage used depends on the location of the cyst. For pseudocysts that occur in the body and tail of the pancreas, a cystogastrostomy is performed. For pseudocysts that occur in the head of the pancreas, a cystoduodenostomy is preferred.
The CADC team is evaluating a new pseudocyst drainage stent and delivery system which may be even safer and more efficient than other stents.
About Pancreatic Cysts
Pancreatic cysts are being diagnosed more and more frequently due to the wide use of cross-sectional imaging techniques, such as CT scans and MRI. These cysts may be diagnosed due to symptoms they are causing, or as incidental findings on imaging tests obtained for another reason. There are many different types of pancreatic cysts, and they vary widely in their potential to become cancerous.
Accurate cyst classification is important to help determine which cysts have malignant potential and require surgery, and which cysts are less of a concern and can be monitored or may not even require follow-up.
Diagnosing And Classifying Pancreatic Cysts

Tools that we use in the CADC to help classify and follow pancreatic cysts include state-of-the-art CT and MRI scans of the pancreas. We also specialize in performing endoscopic ultrasound (EUS), which allows us to obtain detailed visualization of the pancreas and important predictive data regarding these cysts.
EUS also allows us to obtain samples of the cyst, which is then analyzed to help classify the cyst further. When needed, we can also use a special type of endoscopy to help us directly visualize the pancreatic duct. This procedure is referred to as "endoscopic retrograde cholangiopancreatography (ERCP)."
In addition to routine ERCP, we can perform pancreatoscopy (direct visualization of the pancreatic duct) and take targeted samples or tissue biopsies. We are also one of the few centers in the country that performs confocal imaging of the pancreatic duct and pancreatic cysts.
For more about these procedures, visit the Advanced Interventional Endoscopy page.
Treatment Of Pancreatic Cysts
For patients who require surgery, we have pancreatic surgeons on our team who specialize in the treatment of pancreatic cysts. In addition to the standard options of surgery and surveillance, we are also able to provide ablative management of these cysts through the injection of alcohol into the cyst cavity.


